“With sufficient repetition, perception becomes reality”
Short cut to Recommended Reading and Web Links
The Continuous Use of Electronic Fetal Monitors -- 99.8% false positive rate, unable to prevent cerebral palsyIn July 2003 ACOG’s Task Force on Neonatal Encephalopathy & Cerebral Palsy concluded that the obstetrical profession was mistaken about the ability of continuous electronic monitoring and liberal use of cesarean section to reduce the rate of cerebral palsy and other neurological disabilities. [‘neonatal encephalopathy’ is birth-related brain damage] In noting the failure of EFM and cesareans to prevent these complications, the report stated that:
“Since the advent of fetal heart rate monitoring, there has been no change in the incidence of cerebral palsy. …. The majority of newborn brain injury does not occur during labor and delivery. Instead, most instances of neonatal encephalopathy and cerebral palsy are attributed to events that occur prior to the onset of labor."
This ACOG task force report had the endorsement and support of six major federal agencies and professional organizations, including the Center for Disease Control & Prevention (CDC), the March of Dimes and the obstetrical professions in Australia, New Zealand and Canada. It is described as the "most extensive peer-reviewed document on the subject published to date."
The September 15, 2003 edition of Ob.Gyn.News stated that:
“The increasing cesarean delivery rate that occurred in conjunction with fetal monitoring has not been shown to be associated with any reduction in the CP rate......
Only 0.19% of all those in the study had a non-reassuring fetal heart rate pattern.... If used for identifying CP risk, a non-reassuring heart rate pattern would have had a 99.8% false positive rate...." [emphasis added]
An August 15, 2002 report in Ob.Gyn.News stated that:
…performing cesarean section for abnormal fetal heart rate pattern in an effort to prevent cerebral palsy is likely to cause as least as many bad outcomes as it prevents."
.... A physician would have to perform 500 C-sections* for multiple late decelerations or reduced beat-to-beat variability to prevent a single case of cerebral palsy. [* ‘numbers needed to treat’] emphasis added
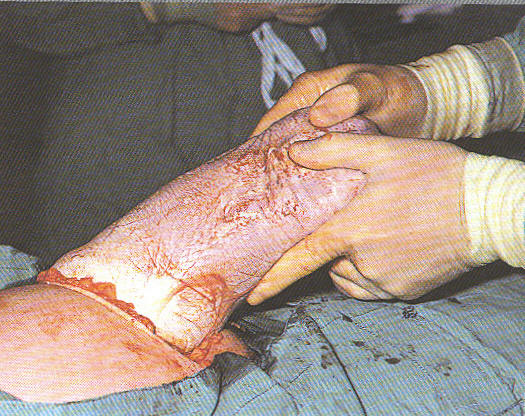
Internal electronic fetal monitor lead attached to baby's head with a small corkscrew needle The only consistent correlation with the continuous use of EFM during labor that has been identified by decades of medical research is a consistent increase in the Cesarean section rate with no improvement in perinatal outcomes.
Understanding Electronic Fetal Monitoring ~ what it can and can't do, how to monitor the baby during labor without the expense or restrictions of this equipment (using intermittent auscultation), so as to avoid the limitations and negative consequences of EFM
Most people incorrectly assume that the electronic fetal monitor is the equivalent of an electrocardiogram (EKG) for the unborn baby. This is a serious misunderstanding of the technology as used for the last 30 year. Electronic fetal monitoring equipment simply provides an elaborate mechanism to count the unborn baby's pulse. The machine transposes the acoustic signal of the baby’s heart rate into a printed paper graph and video display. This permits the educated observer to evaluate a graphic representation of the four auditory markers of fetal well-being – baseline heart rate (110 to 160), variability (should be present 90% of time), accelerations (should be intermittently present) and decelerations (occasional brief decels, especially during pushing, are OK but generally should not be deep, frequent or prolonged).
Over the course of the 20th century, medical science has developed a more sophisticated understanding of fetal heart tone patterns (FHT) patterns, especially in regard to variations and deviations from the normal baseline and their relationship to uterine contractions. It is interesting to note that this method of beat-by-beat auscultation in relationship to uterine activity was the theoretical underpinnings that eventually lead to the development of electronic fetal monitoring equipment. But the original theory and method of fetal surveillance comes from the work of Dr. Joseph DeLee. In his 1924 obstetrical textbook he described counting fetal heart tones during a uterine contraction in twelve, 5-second sampling and then transposing these numbers on to a graphic representation of the uterine contraction. [Principles and Practice of Obstetrics; DeLee, 4th edition, ch. 8, p. 144].
Midwives, physicians and labor room nurses have been listening to fetal heart tone for most of the 20th century, so obviously continuous EFM is not the only way to track the wellbeing of the fetus in labor. However, the way this information was collected in decades past did not usually integrate all four markers of fetal wellbeing, making this an inadequate tool for protecting fetal wellbeing. During the last 20 years a method has emerged to collect the same type of information electronically gathered by EFM, but without the expense or restrictions of this equipment. This equally effective alternative method is called “intermittent auscultation” or (IA) and it is able to detect the baseline rate, heart rate variability, accelerations (if present) and pathological decelerations (if present).
Intermittent auscultation describes a process to gather that same information by listening regularly to fetal heart tones with a fetoscope or an electronic Doppler for one full minute immediately following a uterine contraction and counting in twelve (or more) 5-second samplings to determine the baseline rate. IA also detects the presence of a normal heart rate, normal variability, presence of normal accelerations and absence of pathological decelerations. In the presence of a reassuring pattern such as described above, the likelihood of hypoxic states (i.e., fetal distress) occurring within the next 120 minutes of normal labor is statistically insignificant. ["Fetal Monitoring In Practice" by Dr David Gibbs & S. Arulkumaran, MD; published in the UK]
While IA is more time-intensive (requiring a professional at the bedside), it is equally as effective as continuous EFM for low and moderate-risk labors, with the added benefit of a greatly reduced cesarean rate (4% vs. 26%). This is, in part, because it unhooks healthy mothers from machines and permits laboring women to move around freely. No longer tethered to the bed by electronic wires, the mother is able to change positions frequently, walk, use hot showers or deep water for pain relief and make “right use of gravity”. IA is harmonious with physiological process, which reduces fetal distress and failure to progress and the need for Pitocin-augmentation of labor, pain medication, anesthesia and instrumental and operative delivery.
In spite of the significant benefits of intermittent auscultation, the obstetrical profession generally dismisses the use of IA for what they claim is the “unacceptably great expense involved in providing the one-on-one nursing that is almost mandatory to perform intermittent fetal heart rate auscultation.” [Obstetrics: normal and problem pregnancies, Gabbe et al; 1992, p. 457]. This is a strange objection, since many hospitals bill, and insurance companies reimburse, $400 an hour for the use of continuous EFM, far less than the average L&D nurse’s hourly salary.
Episiotomy Debunked, Revealed as Non-Consensual Surgery
Every five years a new study debunking the routine use of episiotomy is published and then ignored like all the rest. The landmark study establishing the lack of benefit to episiotomy was a paper published in 1983 by researcher and physician, Dr Robert Woolley. When presented with corrective information, the obstetrical professions consistently fails to take corrective action.
The most recent statistics on this ever-so-intimate surgical procedure documented that about a third of women in the United States who gave birth vaginally in 2000 had an episiotomy. That is about 1.3 million unnecessary and painful surgical procedures. In a review published in Ob.Gyn.News on June 1 2005 (Vol. 40 • N0 11), entitled “Routine Episiotomy Offers Women No Benefits or Relief, Review notes longer recovery, some harm”, the situation was described this way by the researchers:
“Routine use of episiotomy for uncomplicated vaginal births provides no maternal benefits and may harm some who would have had lesser injury without a surgical incision, according to a literature review. [..without episiotomy], women were less likely to have severe perineal lacerations and to need suturing, and were more likely to have an intact perineum and to resume sexual intercourse earlier, reported Katherine Hartmann, M.D., University of North Carolina at Chapel Hill, and her associates.”
“The routine use of episiotomy has been standard for years, with apparently limited research to support it,” Carolyn M. Clancy, M.D. … In an interview of Jay Goldberg, M.D., Thomas Jefferson University Hospital in Philadelphia, Dr Goldberg said. “Although episiotomy is among the most common surgical procedures performed on women, it is the only one in which neither informed consent nor patient assent is obtained before performing the procedure.
Physician Using Scissors to Cut a Media-lateral Episiotomy
No practitioner would think of attempting amniocentesis, external cephalic version, cesarean section, forceps-assisted delivery, or vacuum-assisted delivery without first discussing this with the patient; however, cutting a woman's genitalia, usually unnecessarily, is thought to be in the realm of practitioner discretion,” said Dr. Goldberg, who has written extensively on the use of the common procedure. [emphasis added]
None of the studies reviewed found pain to be lessened by routine episiotomy. The evidence showed that the procedure did not protect women against … incontinence, pelvic organ prolapse, and difficulties with sexual function in the first 3 months to 5 years after delivery (JAMA 2005;293:2141-8).
The risk of a woman having an episiotomy during a spontaneous vaginal birth is based more on physician than patient characteristics, according to Jay Goldberg, M.D. ….. board-certified [ACOG-certified obstetricians] cut more episiotomies than did non-certified practitioners [i.e., family practice physicians and professional midwives].
The investigators estimated that about 1 million episiotomies could be avoided annually. They called on clinicians to change their practice patterns, noting that episiotomy use is heavily driven by local professional norms, experiences in training, and individual practitioner preference rather than by variation in the needs of individual women at delivery. [ Ob.Gyn.News; “Routine Episiotomy Offers Women No Benefits or Relief, long recovery, some harm” 06/01/05]
Obstetrics as a prisoner of its own project ~ ever upward, no matter how contradictory the evidence.
If the obstetrical management of a healthy population of childbearing women is to be provided to Americans as a replacement for physiological care, we should be certain that this replacement system uses evidence-based practices. The question is one of efficacy (safety + cost-effectiveness).
The Bible of Science Based Birth Care --
A scientifically researched publication known as ‘A Guide to Effective Care in Pregnancy and Childbirth’ (GEC) by Drs Ian Chalmers and Murray Enkins is the bible of evidenced-based maternity care in the 20th and 21st centuries. It is a compilation of all pregnancy and childbirth related studies published in the English language in the last 30 years. This Internet version of this publication is known as the Cochrane Data Base.
To determine the scientific aspect of current obstetrical care, the Guide to Effective Care identifies six levels effectiveness /efficacy, ranging from the positive end of ‘clearly beneficial’ (category 1) to the negative end (category 6) of ‘likely to be ineffective or harmful’. Using the preponderance of available evidence, Doctors Chalmers and Enkins rated each ‘standard’ maternity-care practice and regularly used medical/ surgical interventions for safety and efficacy. Based on these categories, the GEC cautioned that:
"Practices that limit a woman's autonomy, freedom of choice and access to her baby should be used only if there is clear evidence that they do more good than harm"
"Practices that interfere with the natural process of pregnancy and childbirth should only be used if there is clear evidence that they do more good that harm"
'Mind the Gap' between Science and Practice
As measured by the six categories identified in the Guide to Effective Care, the “standard of care” as presently provided by obstetricians is extremely discordant when measured by scientific principles (both in practice and in the interpretation of scientific studies) and evidence-based practice parameters. Contemporary obstetrics reverses the recommendations of the Guide to Effective Care.
Those caregiver practices recommended as the most beneficial and least likely to cause harm (lists #1, 2 & 3) are the last or least used in contemporary obstetrics.
Instead, those identified as most likely to be ineffective or harmful (lists #4,5 & 6) are the primary or routinely used methods in contemporary obstetrical practice.
This vastly increases the number of medical and surgical interventions used and the complications occurring, both immediately and downstream.
Maternity Center Association Report “Listening to Mothers”
Information on the childbearing woman’s experience of childbirth and the care she received is strangely missing from most obstetrical sources. For that information we turn to the October 2002 report by the Maternity Center Association “Listening to Mothers: Report of the First National US Survey of Women’s Childbearing Experiences” conducted by the Harris Interactive Polling Service. The Maternity Center Association (MCA) of New York City is a non-profit organization established in 1918. It promotes safer maternity care and develops educational materials for expectant parents on ‘evidenced-based’ maternity practices -- that is, policies that are based on a scientific assessment of the safety and effectiveness of commonly used methods and procedures.
The MCA commissioned a survey of healthy mothers with normal pregnancies (no premature or breech babies, multiple gestations, or sick mothers) who gave birth in the last 24 months to track contemporary obstetrical trends and the quality of care received by healthy childbearing women. The full report (some 60 pages long) is available on the Internet at www.maternitywise.com.
MCA Study Concludes ~ No ‘normal’ births in American Hospitals
According to the “Listening to Mothers” survey, 99% of healthy pregnant women did not receive science-based maternity care from their obstetrical providers. The average healthy mom was exposed to 7 or more significant medical interventions and/or surgical procedures during a ‘normal’ labor and birth. The document notes that in the previous 24 months (Oct 2000 to Oct 2002) there were virtually no ‘natural’ births occurring in hospitals. The entire hospitalized population of healthy mothers-to-be were subjected to one or more major interventions.
The only women who had a normal birth without medical or surgical interventions were those who had their babies at home or an independent birth center.
The survey also documented a significant gap between scientific evidence and standard obstetrical practice. Healthy, low-risk women in the United States often receive maternity care that is not consistent with the best research and in fact, is often in direct opposition to scientific recommendations. According the MCA, many people are not aware of the following major areas of concern:
The under-use of certain practices that are safe and effective
The widespread use of certain practices that are ineffective or harmful
The widespread use of certain practices that have both benefits and risks without enough
awareness and consideration of the risksThe widespread use of certain practices that have not been adequately evaluated for safety and effectiveness
According the ‘Listening to Mothers’ survey, the majority of childbearing women did not receive the safer and more satisfactory type of care delineated in the top 3 categories (lists #1, 2, and 3 established as beneficial) and instead were exposed to a plethora of practices in the bottom 3 categories rated as of unknown or unproven effectiveness, unlikely to be effective or known to be harmful.
The survey documented the following statistics are for healthy women at term with normal pregnancies. Intervention rates would be higher for women with medical complications.
93% Continuous electronic fetal monitoring;
86% IV fluids and denial of oral food and water
74% Immobilized or confined to bed due to physician preference,
hospital protocols or the limitations imposed by multiple medical devices
(EFM, IVs, epidural catheter, Foley bladder catheter, etc)
71% Push and deliver with mother lying flat on her back
67% Artificial rupture of membranes
63% Epidural anesthesia
63% Pitocin induced or accelerated uterine contractions
58% Gloved hand inserted up into the uterus after the delivery
to check for placenta or remove blood clots
52% Bladder catheter
35% Episiotomy
24% Cesarean delivery (12.6% planned/12.4% in labor
11% Operative – one-half forceps, half vacuum extractionThe survey population was essentially healthy (95% +/-). However, an astounding 70% of women had some form of surgery performed – episiotomy, forceps, vacuum extraction or Cesarean section.
~ Episiotomy
~ Forceps
~ Vacuum
~ Cesarean SectionMind the Gap ~ an astounding 70% of healthy women had childbirth surgery performed – episiotomy, forceps,
vacuum extraction or Cesarean section, despite the total lack of scientific evidence for the widespread practice.The results from Listening to Mothers survey are confirmed by the data from the Center for Disease Control’s (CDC) National Center for Health Statistics (NCHS) Vol. 47, No 27, on The Use of Obstetric Interventions 1989-97. It documents a steady annual increase since 1989 in each of these obstetrical interventions. A press release dated June 6, 2002 based on the NCHS report “Births: Preliminary Data for 2001” [NVSR Vol. 50, No. 10. 20 pp] for the year 2001 documents a 24.4% CS rate (the same rate as identified by the Listening to Mothers survey). Statistics for the year 2002 show an even higher Cesarean rate – 26.1 in the US and 26.8 in California. http://www.cdc.gov/nchs/releases/02news/birthlow.htm)
As a result of the Listening to Mothers survey, the Maternity Center Association’s recommended:
“ ..more physiological and less procedure-intensive care during labor and normal birth”.
Tort Law and Voluntary Consent
Our tort laws currently force doctors to provide interventionist care irrespective of either the health status of the mother or her wishes. It should be noted that this creates an asymmetrical burden of risk that falls unfairly on the childbearing woman. The mother/baby couple is exposed to the actual pain and potential harm of medical and surgical interventions in order to reduce the risk of a lawsuit against the obstetrician. This is deeply offensive and certainly not consistent with either scientific principles, the ethical premise of medicine “In the first place do no harm” and the legal requirement to obtain voluntary and fully informed consent.
While the medical system gives full lip service to fully informed consent, when the topic is obstetrical interventions, such as induction and especially Cesarean section, the consent process as used today in the obstetrical world does not actually comply with the legal principles of informed consent. For instance, a report on the misuse of episiotomy published in Ob.Gyn.News (June 1 2005 (Vol. 40 • N0 11), entitled “Routine Episiotomy Offers Women No Benefits or Relief, review notes longer recovery, some harm”, one of the experts interviewed noted that. “Although episiotomy is among the most common surgical procedures performed on women, it is the only one in which neither informed consent nor patient assent is obtained before performing the procedure.
And should a woman be perceived as ‘non-compliant’ with obstetrical advice or even just wavering or unsure, wanting to go home and think about it longer or to get another medical opinion, enormous psychological pressure is brought to bear, up to and including threats that a court order may be sought out or that Child Protective Services will be notified. Permission arising out of that kind of power disparity can never be considered to be voluntary and fully informed consent.
The concept of ‘informed consent’ may seem unduly complicated for a layperson. But really it is quite straightforward and ever so helpful to at least be familiar with the basic ideas of permission and informed consent.
The legal theory of informed consent includes the following three aspects:
(1) An acknowledgement that physicians have a duty to obtain informed consent of patients before they perform potentially risky, complex, invasive, painful or experimental medical procedures
(2) That a mentally competent patient has the right to consent or refuse to consent to any recommended medical procedure
(3) That a patient has the right to sufficient information to make that consent meaningful
If a physician treats a patient without any consent, he or she may be liable for battery or an intentional ‘tort’. This applies not only to non-consensual treatment but also when a physician exceeds the scope of the patient’s consent, whether or not the treatment or procedure was properly performed. If a physician obtains a patient’s consent to treatment but does so under duress or trickery, it does not count as truly voluntary or freely given informed consent. This makes the physician vulnerable to charges of battery. If the physician obtains a patient’s consent to treatment but fails to provide sufficient information to make a meaningful decision, the patient may bring legal action for negligence based on lack of informed consent.
Fully Informed Consent Means the Truth, the Whole Truth and Nothing But the Truth…
Generally speaking a physician must disclose all information which is ‘material to the patient’s decision of whether to proceed”, that is, “that information which the physician knows or should know and would be regarded as significant by a reasonable person in the patient’s position when deciding to accept or reject the recommended procedure. This standard does not require a warning for every possible risk [i.e. remote or rare complication] and the physician is not required to give a ‘mini-course’ in medical science. However the patient must be given enough information in lay terms to make a knowledgeable decision regarding the recommended medical procedure.” This includes the risks, complications, expected benefits of the proposed treatment (including likelihood of success) and any alternative to the procedure, including the alternative of no treatment and the relative risks and benefits of not having the procedure. [California Medical Association Document # 0415 – Informed Consent, Jan 2001]
Were we to impose the two clearest, most easily understood and most basic requirements -- “information which the physician knows or should know” and “would be regarded as significant by a reasonable person in the patient’s position when deciding to accept or reject the recommended procedure” the only possible answer would be the truth as it is known to the obstetrical profession through textbooks, journals, trade papers (Ob.Gyn.News) and conferences.
To quote the editor of a well-respected obstetrical textbook (Davis) published in1966, “There can be no alibi for not knowing what is known.” Doctors are formally educated and highly paid to know the scientific literature and be aware of the full spectrum of consequences associated with medical and surgical interventions. It is not unreasonable to expect their advice, both to the public and to individuals, to be objective.
“There can be no alibi for not knowing what is known ….”
Here is a brief list of headlines from contemporary editions of Ob.Gyn.News on the topics identifying physiological pushing as superior to coached or "purple" pushing, harm cased by routine use of episiotomy and the detrimental effects of elective or repeat Cesareans. It easily identifies both what a ‘physician knows or should know’ and what would be considered significant by a reasonable person before giving or withholding permission to be induced, immobilized in bed, medically unnecessary C-section performed, etc:
“Upright Positions Offer Most Room for Delivery” 02/01/02
“Reconsideration of ‘Purple Pushing’ Urged” 03/15/03
“Routine Coached Pushing May Be Harmful” 10/01/04
“Routine Episiotomy Offers Women No Benefits or Relief, long recovery, some harm” 06/01/05
“Induction Linked to Doubling of Cesarean Rate in First-Time Mothers” 01/01/03
“C-Section-Cervical Ripening Link Seen in Women previously delivered vaginally” 06/15/03
“Estimated Fetal Weight Not a Guide for Cesareans” 12/12/01
“C-Section to Prevent Cerebra Palsy: Results May Be a Wash” 04/15/02
“Double-Layer Cesarean Closure May Be Safer” 03/15/02
“C-Section Linked to Stillbirth in Next Pregnancy” 05/15/03
“Maternal Morbidity Rises Sharply with Repeat Cesareans” 03/15/05
“Prior C-Section Assoc. with Worse Outcomes – ICU Admit, postpartum infection” 03/01/05
“Study Shows Elective Cesarean Riskier than Vaginal Delivery” 05/01/04
“Asthma [for baby] Associated with Planned Cesarean” 05/14/03
“Cesarean Birth Associated with Adult Asthma”[for baby] 06/15/01
“Steep Rise Seen in “No [Medical] Risk Primary C-Sections” 01/01/05
“Cesarean Rate Portends Rise in Placenta Accreta” 03/01/01
“ Placental Invasion on the Increase – hike in C-Section may be responsible” 01/15/03
“Placenta Previa, C-Section History Up Accreta Risk” 09/15/01
“Childbirth, Pregnancy Tied to PTSD, Expert Says” 01/15/03
“Offering C-Section ‘On Demand’ Can Be Ethical: ACOG” 12/01/03
Obstetrical Intervention as a Highly Pathological System of Care for Healthy Women
The United States system of medicalized maternity care routinely uses obstetrical interventions on all healthy women who present themselves to obstetrical care providers. According to the MCA “Listening to Mothers” survey of women who gave birth between October 2000 and October 2002, virtually 100% of healthy women who labored under obstetrical management had one or more medical &/or surgical interventions. The average number of interventions per new mother was seven, with an operative rate (episiotomy, vacuum, forceps and/or C-section) of 70%. Data collected by the federal government identified 1.2 million C-section and 1.3 million episiotomies in 2003 or a total 2.5 million surgeries. From the standpoint of iatrogenic ‘risk’, this would put obstetrics into the category of a highly pathological form of maternity care for healthy women with normal pregnancies.
But before we can address the accuracy of this statement from a statistical basis, it is necessary to become familiar with the idea of ‘risk’ as it applies to health care and in particular, to establish the rules generally used in regard to risk in childbirth. We must determine what the status of “very high risk” actually means in terms of numbers of times that something happens in a given population before we can return to the statement that obstetrical care itself is at the highest level of riskiness when used routinely on healthy women.
The basic idea is a mathematical formula generally use for determining risk to childbearing women and their unborn or newborn babies. This method uses the number of occurrences for a specific intervention (such as induction of labor, episiotomy or C-section) or specific complication (such as fetal distress, cord prolapse or hemorrhage) per 10,000 mothers or babies as the measure of risk for that specified occurrence.
In other words, how likely is it that ‘it’ is going to happen to you? – one out of one (100%), one out of ten (10%), one out of a hundred (1%), one out of a thousand (0.1%, one out of a million (0001%). By tracking the number of times that a specific adverse event happened in a population of 10,000 mothers or 10,000 babies, a conclusion can be reached as to whether a healthy women with no other identified risk factors is at very low risk, low risk, moderate risk, high risk or very high risk for having that particular problem befall her during her pregnancy or childbirth.
Here are the actual numbers (taken from the MCA web site www.maternityWise.org):
VERY LOWless than 1 out of every 10,000 mothers or babies
LOW1 to 9 out of every 10,000 mothers or babies
MODERATE10 to 99 out of every 10,000 mothers or babies
HIGH --100 to 999 out of every 10,000 mothers or babies
VERY HIGH --1,000 to 10,000 out of every 10,000 mothers or babies When it comes to biological complications of labor and birth, such as perinatal or maternal death, the physiologically managed group and the obstetrically managed group were virtually identical. From the baby’s stand point; labor and birth are a ‘moderate risk’ activity. About 2 per thousand (20 per 10,000) is the average mortality for babies born to essentially healthy women with normal pregnancies, regardless of the setting (home, hospital or birth center) and regardless of the care provider (midwife or obstetrician).
For women having a vaginal birth, the risk of maternal death is very very low risk – only 1 in 16,666 deliveries. This number includes all women, all pregnancies and all vaginal births -- sick mothers, abnormal pregnancies and the entire spectrum of complications and interventions such as induction and use of forceps. The risk of maternal death associated with Cesarean section is 3 times higher but within the parameters of the risk formula it is not hugely different. Even a Cesarean is within the ‘low’ risk category, at 1 death out of 2,500 (4 per 10,000) for all Cesareans (including emergencies) and 1 out of 5,000 for elective Cesarean sections (or 2 per 10,000).
However, when it comes to the risks of medical and surgical interventions and the immediate, delayed and downstream complications that such interventions generate, there is a huge difference between physiologic and obstetric care. The physiologically managed group (including transfer to obstetrical care and subsequent interventions including Cesarean section) had far fewer intervention by 1/5 to 1/10th the number associated with obstetrical care and yet these mothers and babies enjoyed a similarly good outcome for both.
Virtually a 100% of women under obstetric care (that is one out of one or 10,000 out of 10,000) experienced at least one significant medical intervention. The benchmark for what is a “normal” level of risk for medical interventions n a hospital setting (immobilization in bed, IVs, continuous EFM, artificial rupture of membranes, Pitocin, pain medications, epidural, Foley catheter) is well over 50% or (5,000 out of 10,000).
The risk of surgical interventions are 7 out of 10 or 7,000 out of 10,000. The risk of C-section by itself is greater than one out of four or 2,500 out of 10,000.
The scientific calculation of high-risk states for obstetrical intervention is factually correct. The quality of interventions performed as a facet of 'routine' care does not improve outcomes for either mothers or babies. The quantity of intervention is no longer merely a 'risk' but rather is a regular and permanent facet. This means that interventionist obstetrical care for healthy women is indeed a highly pathological (and expensive) form of maternity care.
Late Breaking News on VBAC by the American Academy of Family Practice Physicians
August 2005
The American Academy of Family Physicians (AAFP) recently published new recommendations regarding vaginal birth after cesarean (VBAC), which differ significantly from the current recommendations of the American College of Obstetricians and Gynecologists (ACOG).
The full text of the AAFP policy document can be found at:
http://www.annfammed.org/cgi/data/3/4/378/DC1/1
Some of the most notable highlights are:
~ TOLAC [Trial of Labor After Caesarian] should not be restricted only to facilities with available surgical teams present throughout labor since there is no evidence that these
additional resources result in improved outcomes.
~ Our recommendation significantly differs from current ACOG policy because we could find no evidence to support a different level of care for TOLAC patients. Without good-quality evidence, we believe that different levels of resources cannot be advocated because their potential for unintended harms cannot be evaluated against their purported benefits.
~ The ACOG policy suggests that one rare obstetrical catastrophe (e.g., uterine rupture) merits a level of resource that has not been recommended for other rare obstetrical catastrophes (e.g., shoulder dystocia, abruptio placenta, cord prolapse) that may actually be more common.
~ Current risk management policies across the United States restricting a TOL after previous cesarean section appear to be based on malpractice concerns rather than on available statistical and scientific evidence."
ACOG currently recommends that an OB and an anesthesiologist should be immediately available, widely interpreted as being on the premises throughout the trial of labor. ACOG recommendations were based on "expert opinion".In contrast, the AAFP recommendations are based on a comprehensive review of published medical studies, a much higher level of evidence for such recommendations.
The ACOG recommendation of having a surgical team immediately available has possibly been one of the biggest limiting factors for hospitals allowing a VBAC, leaving women with limited or no options for avoiding a repeat cesarean section.
The AAFP guidelines certainly give family practice physicians more incentive to allow their patients to have a VBAC than the ACOG policy currently gives an Ob/Gyn.It will be interesting to see how the AAFP recommendations will factor into the current climate, and how useful they may be for women and birth advocates working to change hospital
policies.
C-section most common US hospital procedure study
August 02, 2005 WASHINGTON (Reuters News)
The most common U.S. hospital procedure is the Caesarean section, with 1.2 million of the operations done each year, according to a government report issued on Tuesday.
Caesarean sections cost $14.6 billion in total charges in 2003, the report from the Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project found.
The report, which can be found on the Internet at http://www.hcup.ahrq.gov/ , lists the other top five inpatient hospital procedures:
-- Upper gastrointestinal endoscopy to diagnose ulcers, stomach cancer and other problems, with 712,000 procedures and $14.5 billion in total charges.
-- Catheterization to diagnose heart problems, with 707,000 procedures and $17.3 billion in total charges.
-- Respiratory intubation and mechanical ventilation, with 617,000 procedures and $35.4 billion in total charges.
-- Angioplasty to widen narrowed arteries, with 676,000 procedures and $26.5 billion in total charges.
Anne Elixhauser, an analyst who helped compile the report, said she was initially surprised to learn how common Caesarean sections are. But it makes sense given the number of births, she said.
"There are 4 million babies born every year. Twenty percent or more of them are done by C-section. That is a lot of babies," Elixhauser said in a telephone interview.
"Nearly a quarter of all (U.S) hospital stays are related to pregnancy and childbirth.
Most people don't realize what a big chunk of hospital care that is."Elixhauser said the report, based on data from 38 states representing 90 percent of all hospital stays, is weighted to reflect the total U.S. population.
She said the relative ranking of the five procedures does not vary much from year to year.
Recommended Reading:
The Baby Catcher by nurse midwife Peggy Vincent, CNM;
Expecting Trouble by obstetrician Dr. Thomas Strong, MD;
The Thinking Woman’s Guide to a Better Birth by birth educator and medical researcher Henci Goer, ASPO;
Birthing from Within by nurse midwife Carolyn England, CNM;
Misconceptions by Naomi Wolfe; Perfect Madness – Motherhood in the Age of Anxiety by Judith Warner;
The Oxytocin Factor by Swedish mother and researcher Dr. Kerstin Uvnas MobergWeb sites www.ScienceBasedBirth.com, and www.collegeofmidwives.org // subdirectory “Safety Issues”
Visit the Maternity Association Center web site <www.maternity-wise.org> to download HTML files for “What Every Pregnant Women Should Know About Cesarean Section” and “Listening to Mothers” Survey
Or click on the MCA links directly from here
What pregnant women want to know:
Hot Topics and Downloads:
- How do I choose my caregiver?
- How do I choose my birth setting?
- How will I cope with labor pain?
- How do I get the labor support I need?
- What should I know about cesarean section?
- How can I prevent pelvic floor problems when giving birth?
- Should I choose VBAC or repeat c-section?
Routine Episiotomy Harms Mothers
- Cesarean booklet — a new booklet to help prepare every pregnant woman to make informed decisions about this important matter.
- Continuous labor support — a systematic review finding important benefits and no known downsides is available here.
- Listening to Mothers — for the first time ever, hear what women nationwide are saying about their childbearing experiences.
- Maternity Topics — not sure whether to choose an ob-gyn, family physician, or midwife? Hospital, birth center, or home birth? Confused about vbac vs repeat c-section? See Maternity Topics for help with these and other important maternity decisions.
- Trauma and Loss after 9/11 — a report on lessons learned from experiences of pregnant women, new mothers and maternity caregivers is available here.
Cesarean Section Booklet
- Episiotomy poses harms: Maternity Center Association responds to JAMA 5/2005 study on how episiotomy poses harms and offers no benefits to mothers
- Episiotomy Advice: Advice to mothers on how to avoid routine episiotomies
Maternity Center Association's cesarean section booklet measures the risks of cesarean birth vs vaginal birth. The accompanying chart "Cesearean Birth and Vaginal Birth: How do the risks compare?" complimentary with purchase. Click here to access the booklet.Concerns About Early Epidurals:
Maternity Center Association responds to NEJM study on the effect of labor pain medication timing on c-section:
In the Maternity Center Association Bookstore:
- NEJM 2/2005 Epidural Study: Get help understanding New England Journal of Medicine study (February 2005) on pain medications and cesarean section
- Labor Pain Relief Advice: Read Maternity Center Association's pain relief advice for pregnant women.
- Cesarean booklet — an absolute essential read for every woman looking for the best research about childbirth options and seeking to avoid unnecessary risk during labor.
- A Guide to Effective Care in Pregnancy and Childbirth — want good information about common discomforts of pregnancy, understanding electronic fetal monitoring, or getting breastfeeding off to a good start? The full text of this acclaimed book is available here, in short easy-to-use chapters.
- Birth Atlas Easel Book - Life-size, high-quality, classic photographic reproductions of three dimensional views of a baby's growth from fertilization through labor and birth.
- Growing Uterus Charts - This full color set of poster-sized charts beautifully illustrates the stages of pregnancy.
- Journey to Parenthood: Your Guide Through Pregnancy, Birth & Beyond - Provides families with the information they need to make informed choices about pregnancy and childbirth.
Return to the History of Midwifery and the Conflict with Obstetrical Medicine