American College of Community Midwives |
||
| Report on an ACOG Committee opinion issued May 2001: | 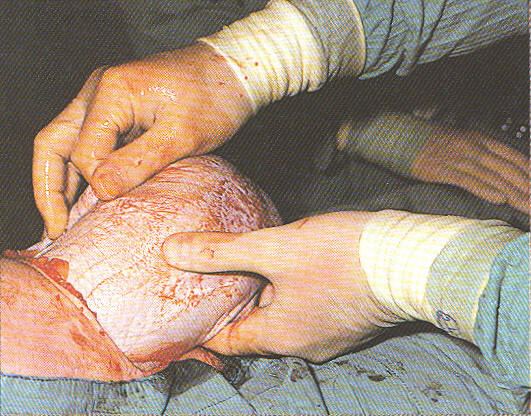 |
Optimal Goals for Anesthesia Care in Obstetrics |
|
General content |
Return to Front Page | |
American College of Community Midwives |
||
| Report on an ACOG Committee opinion issued May 2001: | 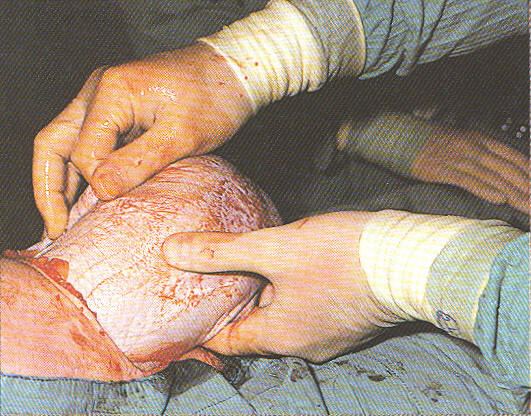 |
Optimal Goals for Anesthesia Care in Obstetrics |
|
General content |
Return to Front Page | |
Synopsis:
The bottom line conclusion on Cesarean "decision to incision" remains 30 minutes. The ACOG / ASA joint committee identified that 50% of all hospital maternity units deliver less than 500 babies a year and are not uniformly able to maintain the perfected standard as proposed by ACOG and ASA. Therefore, they recommend closing the maternity units of smaller community hospitals. This is to better met the practical and economic considerations of the anesthesiologists in regard to their routine and emergency functions. It is not an unreasonable conclusion but is intensely "provider-centric". It would organize all maternity services around the requirements for anesthesia instead of the practical and predictable needs of healthy mothers and their normal unborn or newborn babies.
One can appreciate the desire of any profession to improve their circumstances, perfect their art and reduce the burdens of the job. However, this recommendation did not include any dialogue with those who would be the most affected by them -- the 50% of childbearing families who depend on community hospitals. Important areas of concern to these childbearing families associated with the loss of all community hospital maternity units include the need to drive long distances while in labor and difficulty for friends and family members (including siblings) to visit during and after the birth. This is even more of a problem for the parents if the baby needs an extended stay in the hospital. In particular driving long distances introduces the very real problem of precipitous birth (especially for multips) and/or the complications associated with an attempt to avoid precipitous births by inducing all multips who do not live within a short distance of the hospital.
The following is a report on a joint statement by the American Society of Anesthesiologists (ASA) and the American College of Obstetricians and Gynecologists (ACOG) concerning the issues of "Optimal Goals for Anesthesia in Obstetrics" as it is of concern to both specialties.
They recommend that: "Good obstetric care requires the availability of qualified personnel and equipment to administer general or regional anesthesia both electively and emergently". They further recommend that "The extent and degree to which anesthesia services are available varies widely among hospitals. However, for any hospital providing obstetric care, certain optimal anesthesia goals should be sought."
Specific Conclusions of the Committee included the following:
"Availability of a licensed practitioner who is credentialed to administer an appropriate anesthetic whenever necessary. For many women, regional anesthesia (epidural, spinal, or combined spinal epidural) will be the most appropriate anesthetic." ...... "Availability of a licensed practitioner who is credentialed to maintain support of vital functions in any obstetric emergency"
This conclusion goes on to recommend the "Availability of anesthesia and surgical personnel to permit the start of a cesarean delivery within 30 minutes of the decision to perform the procedure; in cases of vaginal birth after cesarean delivery (VBAC), appropriate facilities and personnel, including obstetric anesthesia, nursing personnel, and a physician capable of monitoring labor and performing cesarean delivery, immediately available during active labor to perform an emergency cesarean delivery" (1)
In this joint opinion by ACOG/ASA, the maternal-fetal risks associated with intrapartum seizures, cord prolapse, placental previa or abruption, etc do not seem to carry the same concern or recommendations as for VBAC labors -- the actual full-time presence of the physician. Perhaps the higher risk is perceived to be that of litigation for the doctor which is associated with VBAC. However, a book written by a physician/lawyer to help obstetricians reduce their liability identified that the absence of the physician during active labor directly contributed to a bad outcome or was a core factor in the problem leading to a severely damaged baby in the majority of 63 cases resulting in multi-million dollar malpractice suits. This applied even when doctors were sleeping in the call room of the hospital as it still depended on the L&D nurse appropriately diagnosing the need for urgent medical intervention and bein bold enough to wake up the physician.
In regard to defining the immediately available personnel and facilities, this joint document recommends that it "remains a local decision based on each institution's available resources and geographic location."
In category IV, the joint committee recommends the:. "Appointment of a qualified anesthesiologist to be responsible for all anesthetics administered. There are many obstetric units where obstetricians or obstetrician-supervised nurse anesthetists administer anesthetics. The administration of general or regional anesthesia requires both medical judgment and technical skills. Thus, a physician with privileges in anesthesiology should be readily available."The committee goes on to further identify that: "Persons administering or supervising obstetric anesthesia should be qualified to manage the infrequent but occasionally life-threatening complications of major regional anesthesia such as respiratory and cardiovascular failure, toxic local anesthetic convulsions, or vomiting and aspiration. Mastering and retaining the skills and knowledge necessary to manage these complications require adequate training and frequent application."
The above information is useful in identifying the common complications of anesthesia and should be included in any "informed consent" provided to laboring women prior to epidural or other regional anesthesia.
Further along in the document it identifies that "Personnel other than the surgical team should be immediately available to assume responsibility for resuscitation of the depressed newborn" This is specifically defined as the need for the "The surgeon and anesthesiologist" (to be) "responsible for the mother and may not be able to leave her to care for the newborn even when a regional anesthetic is functioning adequately." It states that individuals qualified to perform neonatal resuscitation should be able to demonstrate a proficiency in the accurate evaluation of the newborn condition, including Apgar scoring and should be knowledgeable in the pathology of a depressed newborn, including acidosis, drugs, hypovolemia, trauma, anomalies, and infection, and other specific indications for resuscitation
The Joint Committee concluded that "many hospitals in the United States have not yet achieved the goals mentioned previously. Deficiencies were most evident in smaller delivery units. Some small delivery units are necessary because of geographic considerations. Currently, approximately 50% of hospitals providing obstetric care have fewer than 500 deliveries per year. Providing comprehensive care for obstetric patients in these small units is extremely inefficient, not cost-effective and frequently impossible."
The ASA/ACOG Committee recommends that "Whenever possible, small units should consolidate" and that when geographic factors require the existence of smaller units, they should be "part of a well-established regional perinatal system".
This recommendation would only be feasible if healthy women with normal pregnancies were routinely assigned to community-based midwifery care -- client homes or free-standing birth centers -- thus reserving the high-tech tertiary hospitals for complicated pregnancies that are likely to require anesthesia for labor or emergency deliveries.
An important facet of these recommendation addresses the issue of "stand-by" time and payment for anesthesiologists. The committee notes that the "availability of the appropriate personnel to assist in the management of a variety of obstetric problems is a necessary feature of good obstetric care. The presence of a pediatrician or other trained physician at a high-risk cesarean delivery to care for the newborn or the availability of an anesthesiologist during active labor and delivery when VBAC is attempted and at a breech or twin delivery are examples. Frequently, these professionals spend a considerable amount of time standing by for the possibility that their services may be needed emergently but may ultimately not be required to perform the tasks for which they are present." The Committee recommends that: "Reasonable compensation for these standby services is justifiable and necessary."
These "Stand-by" recommendations are very important to VBAC mothers as it makes VBAC care more expensive for the insurer than elective cesarean. The new ACOG recommendations on VBAC, in combination with the paid standby policy of the ASA, addresses the VBAC situation from the legal/economic perspective of the medical profession. But it also effectively eliminates the option of VBAC for many women. The problem here is that a conflict of interest between childbearing women and the professional interests of medicine has not be acknowledged or addressed. Any policies or practices that vastly increase medically unnecessary Cesarean surgery must be given the highest level of scrutiny, which has not occurred in regard to these policies.
The Committee's final conclusion states that "good interpersonal relations between obstetricians and anesthesiologists are important. Joint meetings between the two departments should be encouraged. Anesthesiologists should recognize the special needs and concerns of the obstetrician and obstetricians should recognize the anesthesiologist as a consultant in the management of pain and life-support measures. Both should recognize the need to provide high quality care for all patients."
One hopes that this concern for quality care and patient well-being will bring about a better dialogue between the recipients of anesthesia services and its providers, one that is less provider-centric and more mother-friendly. .
Reference: American College of Obstetricians and Gynecologists. Vaginal birth after previous cesarean delivery. ACOG Practice Bulletin 5. Washington, DC: ACOG, 1999
Bibliography: Committee on Perinatal Health. Toward improving the outcome of pregnancy: The 90s and beyond. White Plains, New York: March of Dimes Birth Defects Foundation, 1993